A couple of Maryland residents who chose to remove their stomachs to prevent stomach cancer say it's one of the best decisions they've ever made.
People with the CDH1 gene mutation have a much greater risk of getting stomach or gastric cancer, and it's a cancer that is hard to treat.
“If you carry this particular gene your risk of stomach cancer over a lifetime is around 60 to 70 percent, and if you put that into context, for women that carry those BRCA gene mutations (which increase the risk of female breast and ovarian cancer), their lifetime risk is about 40 percent,” National Institutes of Health Clinical Center Surgeon in Chief Dr. Jeremy Davis said.
Davis heads a clinical trial at National Institutes of Health, studying the effects of stomach removal for patients who have an inherited risk of stomach cancer. While gastric cancer is not common, it often goes undetected until after it spreads.
“Most stomach cancers arise for reasons we don't really know, though there are environmental factors at play, but David (Fogel) happened to inherit a gene mutation, and patients like David are uncommon, but they are at greater risk for stomach cancer,” Davis said.
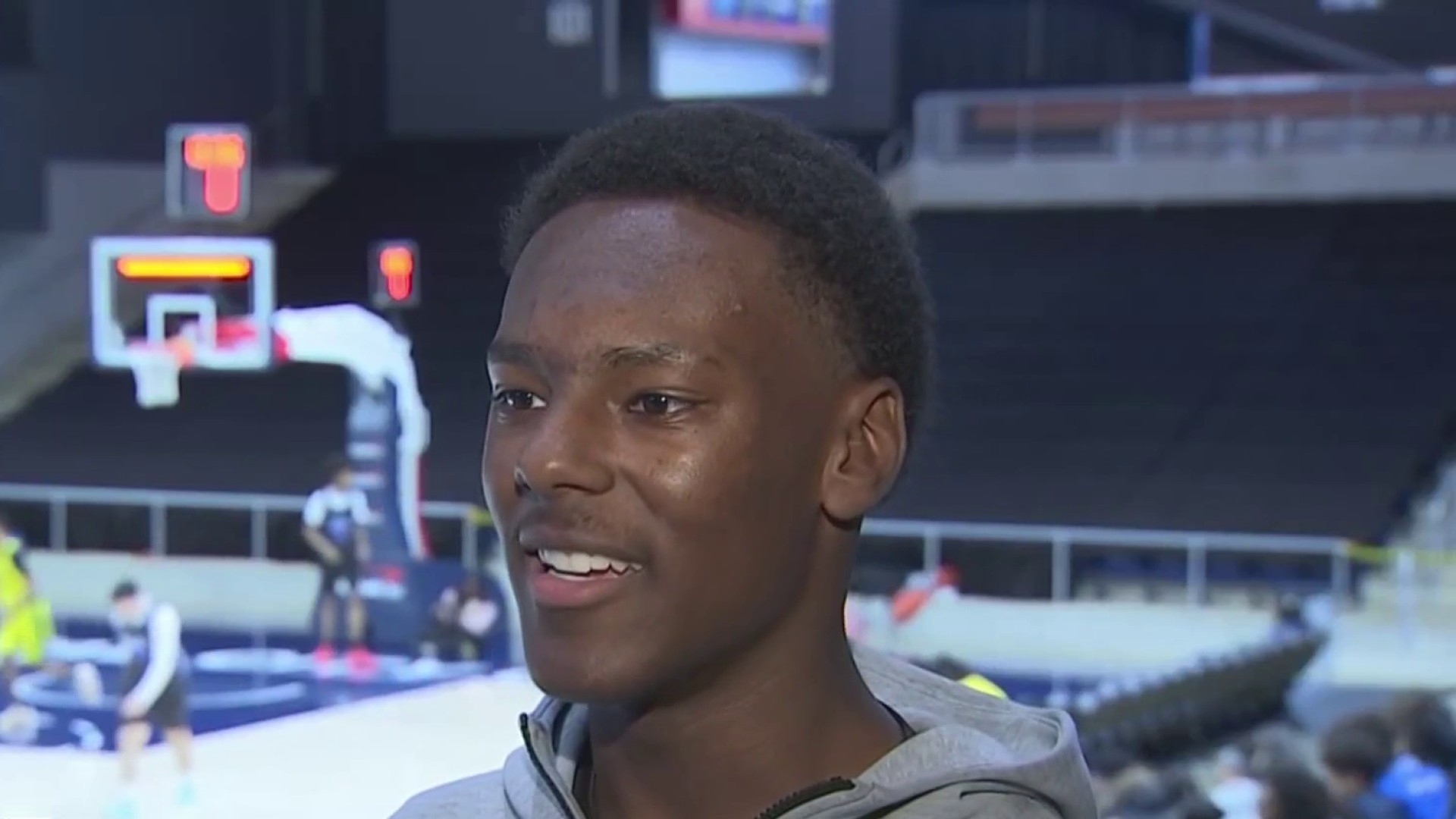
Fogel lives in Silver Spring, Maryland, with his wife and two young sons. When he tested positive for the gene mutation last year at age 40, he knew he had to take action. He had watched his beloved aunt die from stomach cancer.
“Going through that with her and my family, I knew that if there was a way to nip that in the bud and not have to deal with it, it was a bit of a no-brainer,” he said.
Local
Washington, D.C., Maryland and Virginia local news, events and information
Through research he found out about the clinical trial at NIH and he reached out to Davis, who agreed to perform a complete gastrectomy and accept him into the trial. Only a few of these operations are performed around the country each year.
Fogel had his stomach removed in October.
“I was really at peace with the decision,” he said. “I was really calm.”
Once the stomach is removed, the esophagus is attached to the small intestine, which is where food absorption takes place in the body. Adjusting diet is the challenging part.
“I eat things like smoothies, which are great,” Fogel said. “I eat yogurt, avocados.”
He has lost 20 pounds and said he no longer ever feels hungry so he sets his watch to remind himself to eat -- six small meals a day. As his body adjusts, he will be able to incorporate solid food into his diet.
Terri Beach, who works with No Stomach for Cancer, an advocacy group raising awareness of the disease, also tested positive for the CDH1 and underwent the surgery a couple of years ago.
“I've been two years now, post gastrectomy, and everyone said to me, ‘You almost forget what it’s like to have a stomach,’ and it's so true,” she said.
At Fogel’s Silver Spring coffee and vinyl record shop, Bump 'n Grind, Beach told him she got her energy back, gained weight and maintained.
“You know what I like to say is that I was blessed, because we have this knowledge that you and I are going to have a second chance at life,” she said.
By conducting a longitudinal study like the one at NIH, doctors can see how people with this gene mutation do over many years, with or without a stomach, allowing researchers to better understand this cancer.
Reported by Doreen Gentzler, produced by Christina Romano and edited by Perkins Broussard.