The CDC and FDA have recommended a pause in the use of the Johnson & Johnson COVID-19 vaccine to investigate reports of potentially dangerous blood clots that occurred in six women in the days after vaccination.
More than 6.8 million people have received the J&J vaccine in the United States, the vast majority with no or mild side effects. Of these millions, six have experienced the clot, the agencies said, adding that "these events appear to be extremely rare."
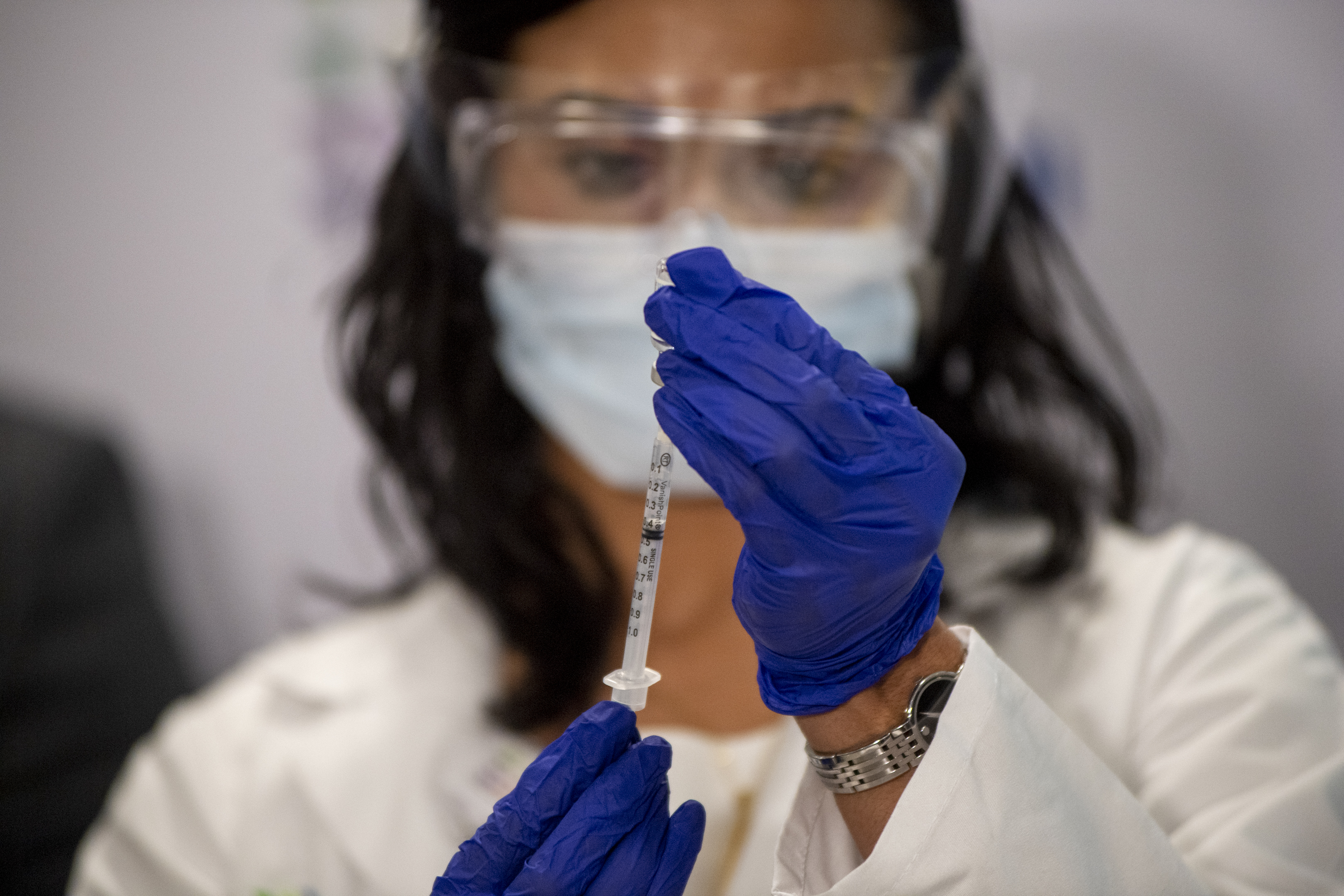
Still, U.S. federal distribution channels, including mass vaccination sites, will pause the use of the J&J shot "out of an abundance of caution," and states and other providers are expected to follow.
Here's what the FDA and CDC say you should do:
We've got the news you need to know to start your day. Sign up for the First & 4Most morning newsletter — delivered to your inbox daily. >Sign up here.
J&J Vaccine - for Consumers
- People who have received the J&J vaccine who are experiencing severe headache, abdominal pain, leg pain, or shortness of breath within three weeks after vaccination should contact their health care provider.
- If you received the J&J shot and have not developed any of the side effects associated with signs of blood clots within three weeks after vaccination, the risk of an adverse reaction is unlikely. Health officials urge patients to continue monitoring for symptoms.
J&J Vaccine - for Doctors
- Health care providers are asked to report adverse events to the Vaccine Adverse Event Reporting System at https://vaers.hhs.gov/reportevent.html
- Ask anyone presenting with the reported side effects if they have recently been vaccinated.
- The FDA and CDC offer this additional warning because of the “unique treatment” required for this type of clot: "Treatment of this specific type of blood clot is different from the treatment that might typically be administered. Usually, an anticoagulant drug called heparin is used to treat blood clots. In this setting, administration of heparin may be dangerous, and alternative treatments need to be given."
What's Causing This Clotting?
It is not yet known why rare blood clots are occurring in some patients who receive the J&J vaccine. The six people who experienced clots were all women between the ages of 18 and 48, with symptoms developing six to 13 days after they received the shot, the FDA and CDC said. They had what's called a cerebral venous sinus thrombosis, or CVST, as well as low levels of blood platelets. The New York Times reports one of the women died and a second woman is hospitalized in critical condition.
Until now concern about the unusual blood clots has centered on the vaccine from AstraZeneca, which has not yet received authorization in the U.S. Last week, European regulators said they found a possible link between the shots and a very rare type of blood clot that occurs together with low blood platelets, one that seems to occur more in younger people.
The J&J and AstraZeneca vaccines are made with the same technology. Unlike the Pfizer and Moderna vaccines, which train the body to recognize the spike protein that coats the outer surface of the coronavirus, the J&J and AstraZeneca vaccines use a cold virus, called an adenovirus, to carry the spike gene into the body. J&J uses a human adenovirus to create its vaccine while AstraZeneca uses a chimpanzee version.