“I can't express enough how dangerous it is in a dental office right now, we have the ability to be asymptomatic and spread this to other people as much as we're looking out for our own safety,” said Cindi Roddan, a dental hygienist, adding, “Everything that we do in dentistry creates aerosols. It is so dangerous.”
High speed drills, ultrasonic scalers and air-water syringes are the tools used in dentistry. According to the Centers for Disease Control they are also potent spreaders of coronavirus because they “create a visible spray that contains large droplets of water, saliva, blood, microorganisms and other debris.”
If a patient is infected with the COVID-19 virus, even if they show no symptoms, those aerosols can contain enough of the virus to infect a dental hygienist, or even the next patient who sits in the dental chair.
Research from the National Institutes of Health and the Centers for Disease Control shows that the particles can survive in the air for hours, and on surfaces for days. “You are spraying into somebody's mouth and literally all of that is going all over the place,” said Roddan.
That’s why Sarah Estopinal, an experienced dental hygienist, was so shocked when she got a text from the dental office where she works, saying: “Please let me know by tomorrow if you are happy and comfortable coming back to a full workload.” Sarah asked, “Is there any new protocol? Is there enough PPE?”
Estopinal’s boss would not do an on-camera interview with NBC Bay Area, but said his practice does have PPE, and that he felt safe opening for business.
In another message to several employees, he wrote, “It really seems you aren’t comfortable coming back. That is fine. I will look for replacements.”
Estopinal is one of three hygienists telling NBC Bay Area they received ultimatums from their employers to return to work. All three hygienists questioned whether those dental practices had new protocols in place to protect both hygienists and patients.
Roddan is not one of those hygienists but said, “It's the financial decision of health and safety versus finances. Will that practice survive? adding, “There are a lot of dentists out there that are ... waiting for guidelines. They're waiting to approve their PPE. But there are others that are not.”
Conflicting guidelines increase the uncertainty. On April 27, California Department of Public Health announced that it was focusing on resuming “our existing health care system,” and it included “routine dental services” among the procedures that could be restarted.
Ten days later, CDPH issued a new directive with many more specific requirements, such as pre-screening of patients to make sure they don’t have COVID-19 symptoms, stocking a minimum 2-week supply of PPE for dentists and staff, and face masks or cloth coverings for all patients in the waiting room to minimize transmission. Meanwhile, CDC guidance says, “Postpone elective procedures, surgeries, and non-urgent dental visits.”
“There's so many different hands on this in the soup,” said Michael LaFlamme, a dental hygienist who works with the California Dental Hygienists Board. “Counties are saying one thing, states are saying another, the federal government, the CDC or OSHA saying something else,” said LaFlamme, and those differing directives are creating potentially hazardous situations as some dental practices scramble to reopen their businesses.
“A lot of these private practice offices want to re-start and they're really crunched up against leases and rent,” said LaFlamme, adding “but I think they risk litigation down the road from their own employees if they push this a little too fast.”

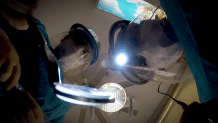
In San Francisco, Dr. Fabiola Lara showed what it takes to perform dental work during the COVID-19 crisis. She’s installed barriers, stocked up on PPE, and outfitted her staffers with what look like space suits.
“It’s still the same person underneath!” said Dr. Lara. Her office is only focusing on dental work that addresses pain or underlying conditions. “We want to make sure that those urgent patients don’t turn into emergency care,” she said.
For now, the practice is not doing cosmetic work, and avoiding most routine procedures. Dr. Lara said she would never make her employees choose between their jobs and safety. “One thing I remind myself is that I have a family to go to. My staff has a family to go to. The patients have a family to go to.”
Dr. Yolanda Mangrum, a dentist with the Petaluma Dental Group, and also an industry leader who is launching a nationwide accreditation process for dental practices said, “If people are scared to go to the dentist, their overall health suffers.”
A University of Illinois study noted a relationship between a healthy mouth and cardiovascular disease, diabetes, even pregnancy complications, although the researchers said the cause and effect was not completely understood. Working with Fortune Management, the dental consulting group, Mangrum and a nationwide team of dentists have developed an accreditation handbook which they say will go beyond any federal, state or county safety requirements. The plan includes protocols for screening patients for COVID-19 well before the dental appointment, leaving time for disinfection and sterilization of the appointment room, and evaluating hygienists for risk factors.
The California Dental Board and the Dental Hygiene Board agree that preventative dental care can resume, as long as guidelines are followed. “For dental offices, I think that the best thing to do would be to have good, clear communication with your staff,” said LaFlamme, “To have everyone talking and see each other and vet out what they would feel they need to have in place to restart work.

